Hey Ladies, Listen up...
Let's talk about something that is very important! Today, we are going to talk about something that we most often overlook, especially as young women, The Well Woman Exam. In this post, I will attempt to answer some of the questions you might have regarding this topic, and if any questions are left unanswered, feel free to ask in the comment section or in a private email message...
What is a well woman exam?
The well woman exam is the time for your health care provider to screen you for potential reproductive health problems, to answer your questions, and to discuss your concerns.
When should you have the exam?
It is important that you have exams regularly so that any problems you may have can be treated early, when they are easier to cure and have caused less damage.-
If you are sexually active or over the age of 18, you should have a well woman exam once every year.
-
You may need more frequent exams if you plan to become pregnant soon, have a history of sexual health problems, or have a mother or sister who developed breast cancer before menopause.
-
You should have an exam immediately if you detect a lump or other unusual change in your breast or have symptoms of a sexually transmitted disease.
-
You should have an exam before starting on hormone therapy if you are menopausal.
-
You should have an exam immediately if you are experiencing bleeding outside of your normal menstrual period.What will happen during the exam?A complete well woman exam has four parts.
-
Basic History and Physical. Your health care provider will ask you a few questions about your sexual, medical, and family history and then will perform a very basic physical exam to check your overall health. Make sure it includes measurement of weight and blood pressure, as they can influence menstrual cycle, pregnancy, and contraceptive or hormone replacement choices. If you are wheelchair bound, the weight of your wheelchair is subtracted from the total to calculate your weight. If you are taking any herbs, vitamins, or nutritional supplements, be sure to tell your health care provider, as some of them can affect your menstrual cycle and hormone balance.
-
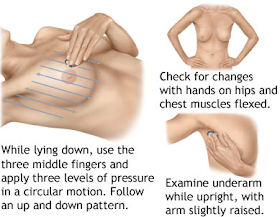
Breast Exam. This is important, because the belief that only older women have breast cancer is a myth. Breast cancer can happen to men and women, even while they are young! When you go for your well exam, your health care provider will inspect and press on your breasts and your arm pits while your arms are in various positions. If your arm mobility is limited, tell your practitioner so that you can find a position that is comfortable for you. You can also do a routine breast exam in the comfort of your home once a month, using the guidelines in the images below. Let your partners help you too! You are looking for lumps, changes in appearance of your breasts/skin, and bleeding or discharge from the nipples. A general rule, if it is round, moves and hurts chances are it is benign versus if it fixed, doesn't hurt and has irregular boarders!
-
Pelvic Exam with Pap Smear. Your health care provider will examine your reproductive organs for problems and check you for cervical cancer. This exam is described in detail below.
-
Contraceptive Counseling. Your health care provider will discuss what, if any, contraceptives you wish to use. Contraception becomes even more important if your periods are becoming less regular as you approach menopause because determining the time of ovulation (release of an egg) and greatest fertility will be less reliable. If you are using hormonal contraception, such as the pill or Norplant, your periods will not stop as menopause approaches. Your health care provider will need to determine when to switch you to lower dose hormone replacement therapy, either by testing blood levels of follicle stimulating hormone (FSH) after a period of hormone withdrawal or by choosing 51 as the most likely age for menopause.
-
Menopause and Midlife Counseling. If you are over age 45 or having perimenopausal symptoms, your health care provider should discuss the risks and benefits of your using hormone replacement therapy (HRT) to restore the estrogen and progesterone that decrease toward menopause. You should be fully involved in the decision making process. He or she should also discuss lifestyle habits that affect the perimenopause transition period. These include smoking cessation, physical exercise, proper diet, especially adequate calcium, vitamin D, and vitamin E, weight maintenance, and stress reduction. If your health care provider automatically assumes that HRT is unsafe for you because of your disability, seek a second opinion. The benefits of using HRT for you may outweigh the risks, especially if you at high risk for osteoporosis (fragile bones) or heart disease. A bone density test should be ordered if you are at risk for osteoporosis, as many women with mobility impairments are. You should also report any increased problems with bladder function or vaginal dryness.
-
Laboratory testing. Standard urine and blood screens should be done. If you are over 45, when heart disease and under active thyroid become more common, serum cholesterol levels and thyroid testing should be included.
What are a pelvic exam and a pap smear?
During the pelvic exam, your health care provider will examine your reproductive organs, including your ovaries, uterus, cervix, vagina, and vulva. The cervix is the portion of your uterus that protrudes into your vagina. Cancer can develop in your cervix. A pap smear is a sample of cells from your cervix to screen for cancer. Because most cervical cancers grow very slowly and can be treated successfully if they are found early, it is important that you have yearly pap smears. Some women mistakenly believe that they no longer need pap smears after menopause. You are still at risk for cervical cancer after your menstrual periods stop. Women over age 60 account for more than 40% of deaths from cervical cancer in the United States. An annual pelvic exam is still needed even if your uterus and both ovaries have been removed, to detect precancers in the vagina and any remaining cervical tissues. The steps in the pelvic exam are as follows.To view the cervix, your practitioner must insert a sterile instrument called a speculum into your vagina. The speculum is made either of plastic or metal. If you have a spinal cord injury, then the pressure or the cold of a speculum can cause you to have problems with autonomic dysreflexia. Be sure that your health care provider understands that this phenomenon can occur, and that she needs to gently insert a warm speculum. Some uninformed health care providersfalsely assume that because you have little sensation, they do not need to use this kind of care. If, at any time, you start feeling sick, sweaty, or dizzy during the exam, ask your health care provider to stop immediately. Those feelings are not normal.While the speculum is in place, your health care provider will perform a pap smear by gently scraping some of the cells from your cervix, and will send the sample to be tested for precancerous or cancerous cells. Your health care provider will notify you of the results of the test and discuss further treatment if a problem is found. You should call the health care provider if you have not received any results within a few weeks of your exam.Your health care provider also may take a sample of the mucus around your cervix so the mucus can be tested for vaginal infections and sexual transmitted Diseases (STDs) such as herpes, gonorrhea, human papilloma virus, and chlamydia. It is possible to have STDs without symptoms. If your health care provider does not routinely take a specimen for these tests, you may ask that it be done -- especially if you have symptoms such as a rash or vaginal discharge, or concerns about your sexual partners.Finally, your health care provider will feel your uterus and ovaries. Wearing an examination glove, she will insert one or two lubricated fingers into your vagina and then press down on your lower abdomen with her other hand. To make you feel more comfortable during your exam, you can ask for another woman to be in the room to reassure you. You can ask the health care provider to tell you what she is doing. She may even place a mirror so you can see what is happening.The pelvic exam is particularly important for women over age 40, when the risk of ovarian and uterine cancer are higher. Avoid using talcum powder between your legs, as it has been associated with getting ovarian cancer. Unusual thickening of the endometrium (lining of the uterus) may indicate uterine cancer, particularly if there is also abnormal uterine bleeding. In this case, examining a specimen of cells from the endometrium will detect any abnormalities.The pap smear is important to screen for changes in your cervix that may lead to cancer, that are due to infection with the Human Papilloma Virus (HPV) types 16 and 18. The new recommended guildelines for pap smear screening is as follows;- Under 21: No Pap smear necessary, regardless of sexual activity.
- 21-29: Pap smear every three years.
- 30-65: Pap smear every three years, or a Pap smear and HPV test together every five years.
- Over 65: No screening if there is no previous history of cervical cancer.
The test result is reported as normal and abnormal. Please note that an abnormal pap test or diagnosis with HPV is not the end of the world. Your doctor will take further steps to ensure that the progression to cervical cancer is prevented.REMEMBER: Early Detection Saves Lives!!Information reference: http://www.bcm.eduImage sources: healthywomanusa.com, plexusglove.com, 2snapsandaswirl.com, americanbedu.com, tips-healthy.com, healthy.kaiserpermanente.org, urbanewomen.com -






Omg thanks Gucci! But biko that pap smear is painful!!!!!!!!! Ok bye. Lol
ReplyDelete